Pressure Ulcers
What is a Pressure Ulcer?
Anyone can develop a pressure ulcer. Researchers say that every year, about 2.5 million Americans develop a pressure ulcer. People who are elderly, immobile, or bedridden are most at risk of developing a pressure ulcer. A pressure ulcer occurs when prolonged pressure reduces or cuts off blood flow to your skin. A pressure ulcer can start to develop in as little as two hours. The skin breaks down, forming an injury to the skin.
What are other names for Pressure Ulcers?
- Bedsore
- Pressure sore
- Pressure injury
- Pressure wound
- Decubitus
What Causes a Pressure Ulcer?
Pressure ulcers are more likely to develop when there are one or more of the four causes listed below.
Causes of pressure ulcers include:
- Pressure: Constant pressure on a part of your body that lessens the blood flow to the tissues
- Moisture: Urine, stool, perspiration, and wound drainage all contribute to an increased risk of pressure ulcers.
- Friction: This is when two forces rub together. As an example, consider skin rubbing against bed linen.
- Shear: This occurs when two surfaces move in opposing directions. For instance, suppose a bed is elevated at the head and a person slides down. The skin over the tailbone remains in place as the tailbone moves downward, effectively pulling the skin in the opposite direction.
Who is at Risk for Pressure Ulcers?
Anyone can get a pressure ulcer. Children and adults with certain long-term health problems are more likely to get pressure ulcers. People who can’t move around much or at all, like those in wheelchairs or who can’t get out of bed, are at very high risk.
These chronic health conditions include:
- Cancer
- Dementia or Alzheimer’s Disease
- Diabetes
- Heart failure
- Malnutrition
- Spinal cord injuries
- Cerebral Palsy
What Parts of the Body Do Pressure Ulcers Affect?
Pressure ulcers occur commonly over bony areas; however, they can develop anywhere on the body if there is prolonged pressure.
Common locations of pressure ulcers on the body include:
- Tailbone
- Hips
- Heels
- Elbows
- Buttocks
- Back
- Ankles
- Ears
- Back of head
What are the Stages of Pressure Ulcers?
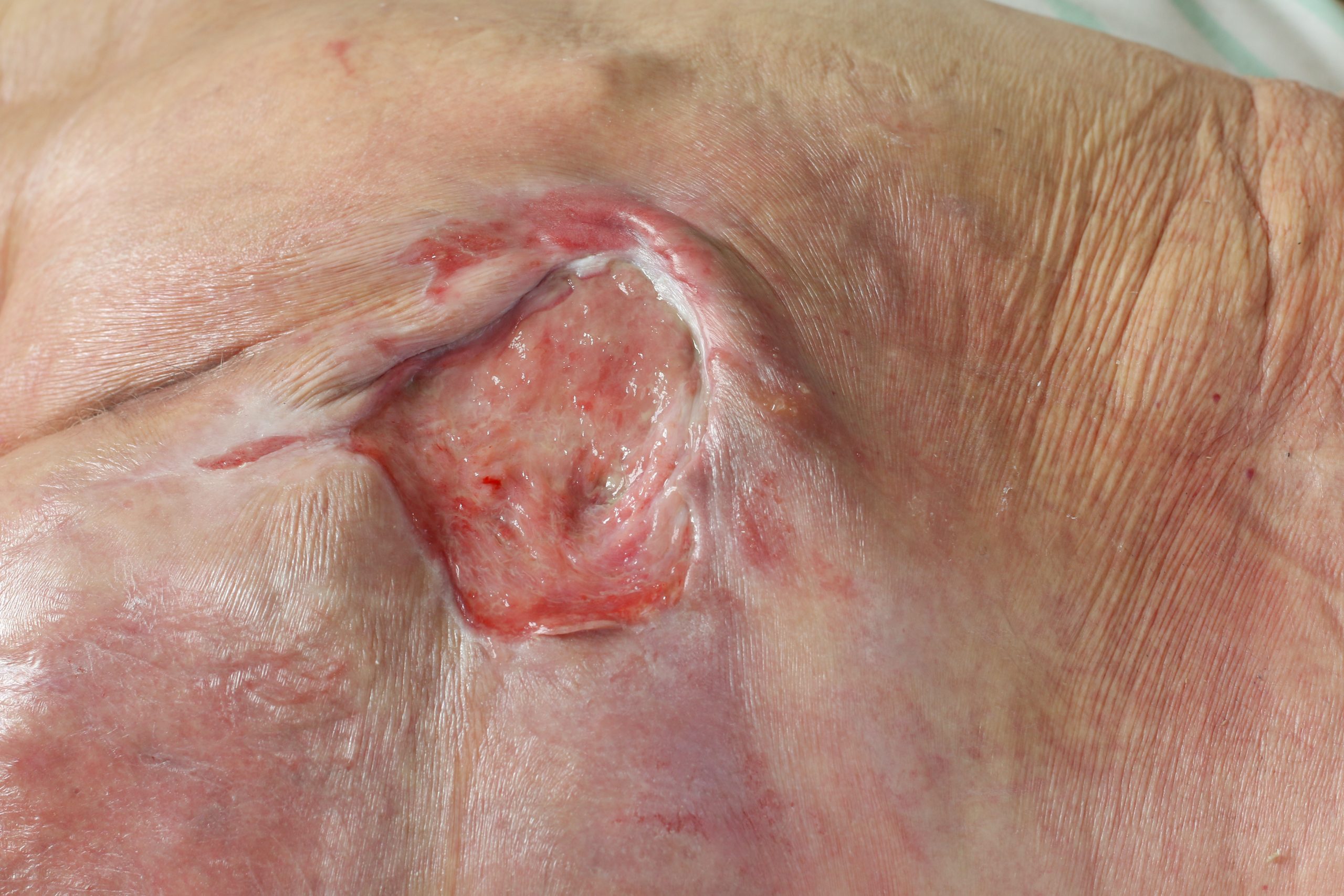
Always notify your doctor or nurse practitioner of any persistent red areas or wounds on your skin. Pressure ulcers may progress through different stages. The worst stages (stages 3 and 4) make you more likely to develop an infection that can be life-threatening. If you develop fever, chills, foul-smelling drainage from the wound, pus, pain, or swelling, notify your doctor immediately. Your doctor may need to use a scalpel to remove dead tissue from deeper ulcers such as Stage 3 or Stage 4 pressure ulcers.
Pressure ulcer stages include:
- Stage 1: Your skin appears red or pink, but there is no visible wound. People with darker skin tones might find it harder to notice a color change. Your skin may be tender to the touch, warmer, or softer.
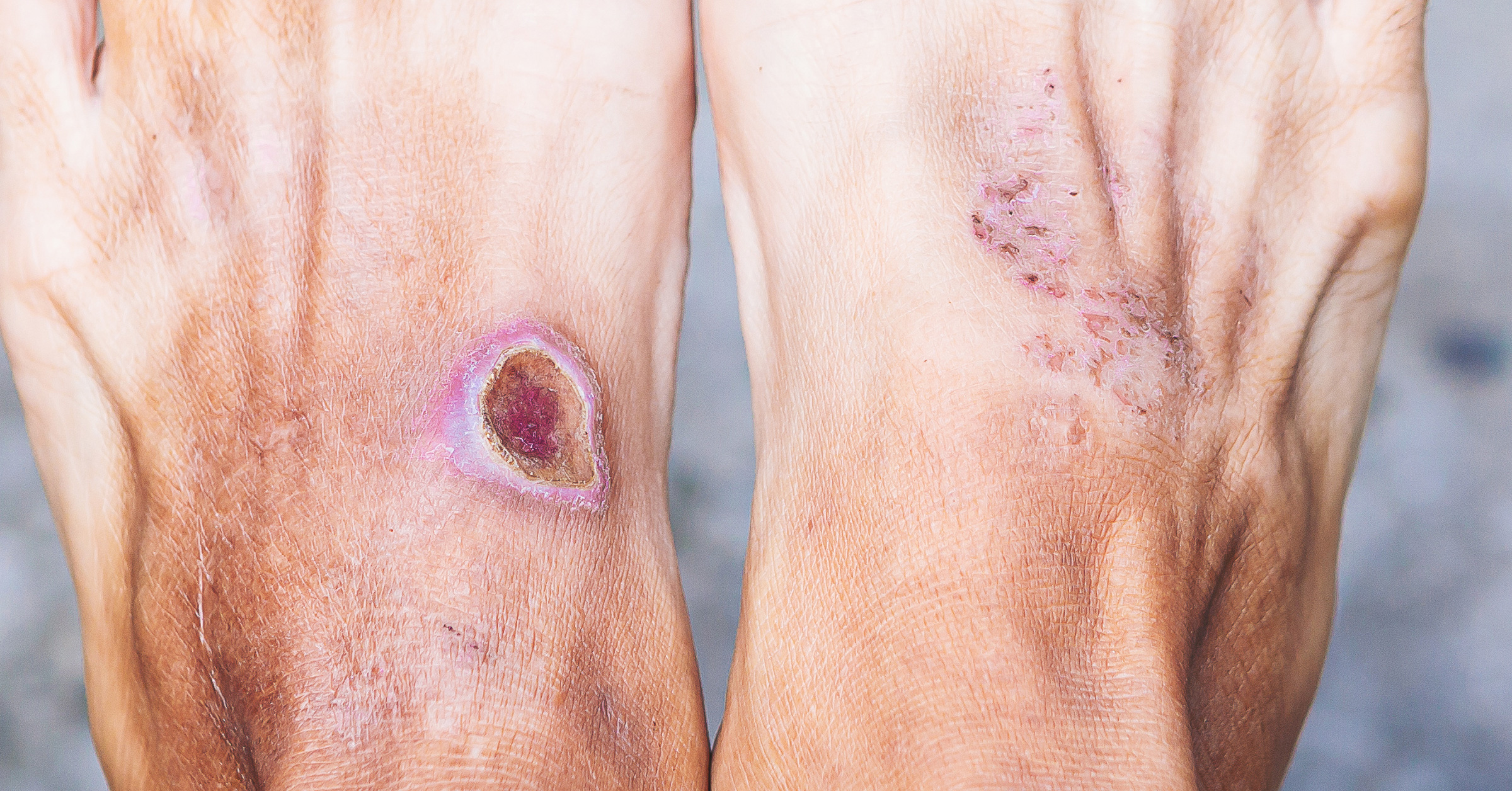
- Stage 2: There will be a shallow crater-like wound with a pink or red wound color base. Blisters are possible.
- Stage 3: A noticeable wound will be visible in the fatty layer of your skin tissue.
- Stage 4: A deeper wound had developed through all three layers of skin. There may be muscle, tendon, or bone present.
- Deep Tissue Pressure Injury: This injury is closest to the bone and may not be visible in its early stages.
How are Pressure Ulcers Treated?
Pressure ulcers can be difficult to treat at times. Reducing pressure on the wound site with frequent turning and position changes is critical, as is treating the wound itself, which includes cleansing the wound and applying the treatment. It is very important to eat a healthy diet to rebuild tissue. Consuming adequate protein can help a pressure ulcer heal.
To treat a pressure ulcer, you or your doctor may:
- Wash your hands to prevent infection.
- Cleanse the wound with AMERIGEL® Saline Wound Wash.
- Apply a layer of AMERIGEL Hydrogel Wound Dressing with a gloved finger or tongue depressor. This dressing is appropriate for pressure ulcers in stages 2 through 4, as directed by your doctor.
- Cover your wound with a special bandage, like an AMERX® Bordered Gauze Dressing. Your wound should be covered in order to heal properly. Wounds that are exposed to air heal more slowly because the surface cells dry out, and as a result, they are more susceptible to infection.
- Change your wound dressing daily, repeating steps until it heals.
NOTE: If you are experiencing any symptoms suggestive of a medical emergency, always contact a physician or seek urgent care immediately.